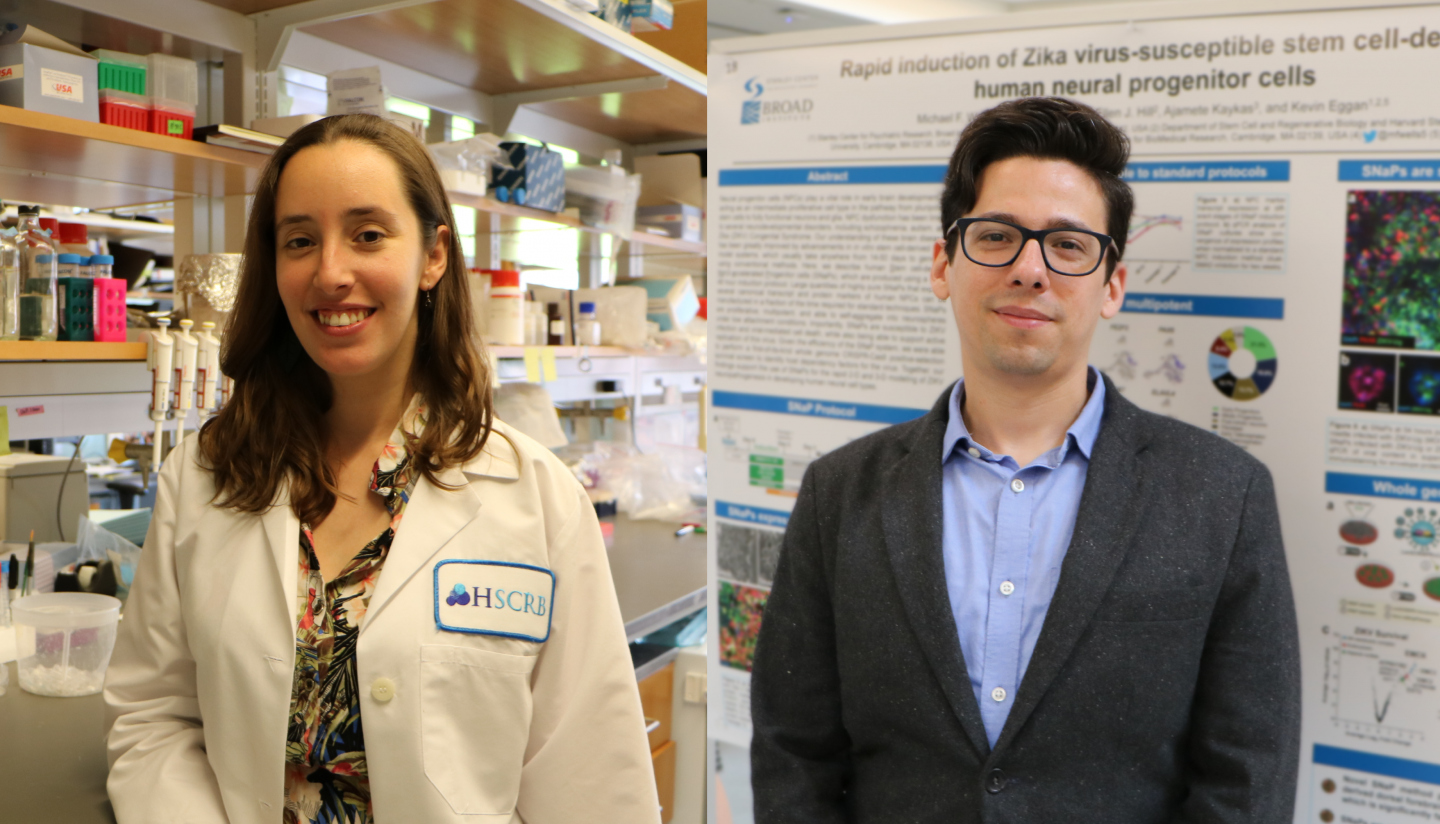
Two postdoctoral fellows at the Harvard Department of Stem Cell and Regenerative Biology (HSCRB) have been recognized for their outstanding research in neuroscience.
Daniela Di Bella, Ph.D., a member of Paola Arlotta’s laboratory, has been named to the Pew Latin American Fellows Program in the Biomedical Sciences. The program provides postdoctoral training support to scientists from Latin America.
Michael Wells, Ph.D., a member of Kevin Eggan’s laboratory, has been selected to participate in the Linton-Poodry SACNAS Leadership Institute. Offered by the Society for Advancement of Chicanos/Hispanics and Native Americans in Science (SACNAS), the institute trains the next generation of scientific leaders. Wells has also been selected for the Burroughs Wellcome Fund’s Postdoctoral Enrichment Program, which supports the career development of underrepresented minority fellows.
Both researchers are setting their sights high: use large-scale data to improve our understanding of how the brain develops. Di Bella will zoom in on the mouse embryonic brain, collecting high-throughput data on individual cells as they develop. Wells plans to study neurodevelopmental disorders, not just with the few human cell lines that are conventionally used, but with dozens or even hundreds of different human cell lines.
Answering old questions with new technology
Di Bella joined HSCRB last fall, having completed her Ph.D. at the Leloir Institute in Argentina. Her move to the department was a natural next step for someone driven to understand the brain during development.
“The developmental neuroscience community in Argentina is small,” Di Bella said. “I felt like an outsider at neuroscience meetings because there weren’t many developmental biology researchers. Here in the Boston area, the field is incredibly big and there are lots of people to learn from.”
In the Arlotta laboratory, Di Bella plans to study how neurons differentiate in the cerebral cortex — the region of the brain responsible for thinking and consciousness — in mouse embryos. That is, she will study how different types of neurons are produced in the developing brain over time.
“The brain is a complex apparatus, but it originates with very simple cells and their instructions,” Di Bella said. “I think that’s fascinating.”
Di Bella plans to analyze gene expression in single cells in the developing cortex, using high-throughput transcriptomics.
“Neuron differentiation has been studied for a long time, but the specific question of how different neurons are produced sequentially — how the switch between neuronal types occurs — has eluded us,” said Di Bella. “I’m excited to apply this new high-throughput sequencing technology to these old questions and try to understand them in more detail.”
Improving cell models of neurodevelopment
When Wells joined HSCRB in 2016, news headlines were dominated by the Zika virus outbreak in Latin America. As the World Health Organization declared the epidemic a public health emergency, Wells was one of many researchers spurred to study the disease and develop interventions.
“Most of my family is from El Salvador and Guatemala, so the outbreak hit close to home,” said Wells. “I immediately got involved with a project to study how the Zika virus infects neurons undergoing early development.”
These so-called neural progenitor cells (NPCs) proliferate extensively in the embryonic brain, so infections during pregnancy can result in microcephaly — where an infant’s head is much smaller than expected.
Over a few short months, Wells used human induced pluripotent stem cells (iPSCs) to grow two- and three-dimensional cultures of NPCs. He used the cell models to study the role of the AXL surface protein in virus infection, but recognizing limitations, soon turned his attention to making the method of producing NPCs faster and more efficient.
“I was frustrated with the long and inefficient protocol to convert iPSCs to NPCs,” said Wells. “I thought it was important to have a reproducible method that could be used with many different iPSC lines.”
Wells has developed a new protocol that cuts down the time to make human NPCs from iPSCs from a couple of weeks to a couple of days. Now, he can expand his investigation beyond Zika virus infection to other neurodevelopmental diseases, including autism.
“NPCs are not just useful for studying Zika — they’re one of the most important cells for the development of the brain,” said Wells. “My Ph.D. background is in studying psychiatric and neurodevelopmental diseases, so I’m applying my NPC method to investigate different cell models of autism.”
Autism is such a complex disorder, with such a broad range of symptoms and causes, that studying it in the laboratory is extremely challenging.
“Previously we could only test cell lines from two or three patients at a time,” said Wells. “I’m aiming to run assays on dozens or hundreds of cell lines at once, so that we have a more complete picture of what’s happening in this disease.”