Research led by stem cell scientists at Harvard University points to a potential new biomarker and drug target for amyotrophic lateral sclerosis (ALS), a neurological disease that is difficult to diagnose and treat. Published in Nature Neuroscience, the study used stem cell models of human motor neurons to reveal the gene STMN2 as a potential therapeutic target, demonstrating the value of this human stem cell model approach in drug discovery.
Diagnosing and treating ALS
Patients with ALS experience the loss of motor neurons and progressive paralysis. Following a long diagnostic journey, most do not survive past five years. Two ALS drugs have been approved by the U.S. Food and Drug Administration (FDA), but they act only to slow the disease.
In addition to a cure – or even a treatment that is effective for more ALS patients – a robust test for ALS is sorely needed. For that to happen, scientists need to find a reliable biomarker of the disease.
TDP-43: a hallmark of ALS
About 10 years ago, scientists found aggregates of a protein called TDP-43 in post-mortem neurons from ALS patients. This protein should have been in the nucleus of those neurons, but instead it was being flushed out, and building up in the cytoplasm.
Clearly, some of the genes at work in the trash-disposal system of neurons (called the proteasome) were interacting with TDP-43 in a way that led to ALS. But which genes are involved, and what they are doing, has not been known.
The gene that encodes for TDP-43 can be mutated to trigger ALS. It is passed on to future generations, who then develop either ALS or, in some cases, frontotemporal dementia (FTD). Since TDP-43 aggregates were discovered in ALS patients, they have been well known as a hallmark of the disease.
What the researchers did
TDP-43 is one of many proteins that binds to RNA, which is responsible for transmitting genetic information and translating it into a concise recipe for a given protein, for example part of a growing neuron.
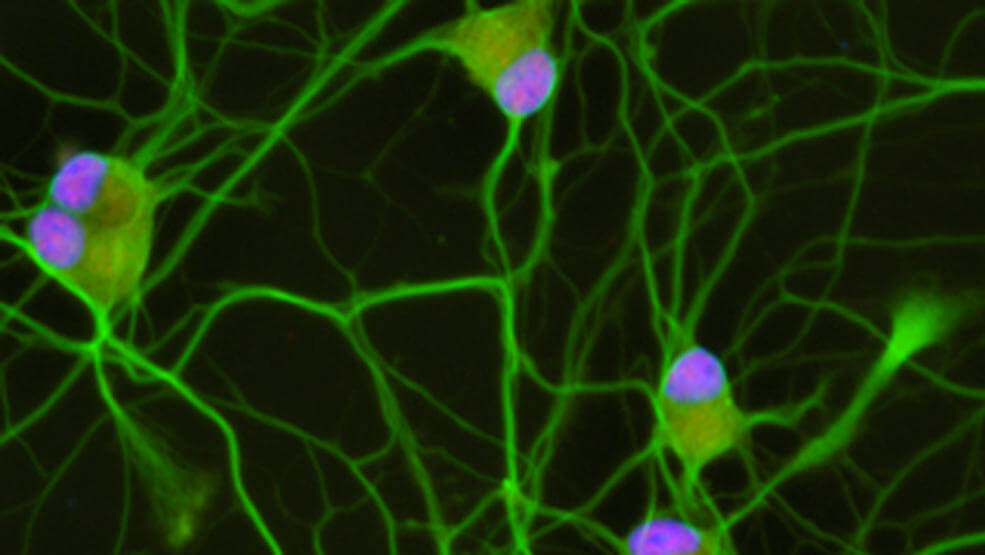
The researchers set out to identify, for the first time, all the possible types of RNA that are regulated by the TDP-43 protein in the context of human neurons. Until now, studies like this have only been carried out in mice and cancer cell lines.
Next, the researchers looked at what happened to each gene when they manipulated TDP-43. They reduced the levels of TDP-43 protein in human stem cell-derived motor neurons. Then, using RNA-sequencing, they analyzed how gene expression changed in these cells.
What they found
Among the thousand or so genes that changed when TDP-43 was manipulated, one stood out: Stathmin2 (STMN2), a gene that is important in neural outgrowth and repair. STMN2 changed consistently in step with TDP-43.
“Once we had a connection between the TDP-43 and the loss of this other critical gene, STMN2, we could see how a motor neuron might begin to fail in ALS,” said Joseph Klim, postdoctoral fellow in the Harvard Department of Stem Cell and Regenerative Biology (HSCRB).
“With the discovery that our human stem cell model had predicted exactly what was happening in patients, Joe went on to test in this system whether fixing Stathmin2 could rescue the motor neuron degeneration in our dish caused by disturbing TDP-43. In a beautiful series of experiments that I believe provide great hope for patients, he went on to show this was exactly the case: rescuing expression of Stathmin2 rescued motor neuron growth,” said Kevin Eggan, Professor of Stem Cell and Regenerative Biology at Harvard University and principal faculty in the Harvard Stem Cell Institute (HSCI).
The culprit
The researchers observed that without TDP-43, STMN2’s perfectly read protein-making instructions turn into nonsense.
“We discovered that when TDP-43 levels are diminished in the nucleus, a cryptic exon is spliced into STMN2 messenger RNA. That basically deletes its instructions for making functional protein,” explained Klim. “It becomes impossible for STMN2 to create a vital component for repairing or growing motor neuron axons.”
Double- and triple-checking
The next step was to see if their findings reflected the reality of a patient’s biology. Because it is not possible to access the affected cells in living patients, they obtained data from a small number of RNA sequencing studies that used post-mortem samples from ALS patients.
Those rare datasets, compared with controls, echoed the team’s original findings in human stem cell models. The data from ALS-patient spinal cords mapped to the cryptic exon, but data from the controls did not.
Why it worked
In neurological disease, findings in mice rarely translate to humans. The Eggan laboratory uses human induced pluripotent stem cells (iPS cells) to create models of neurological disease. In this study, the human model was crucial: the cryptic exon involved is not observed in mice.
“This would never have been identified in a mouse study, because the mechanism is most likely a quirk of human biology,” said Professor Eggan. “We could predict that TDP-43 is targeting STMN2 RNA only because we have these precise, human cellular disease models. Being able to validate that with RNA sequencing data from patients was incredibly exciting. It shows how relevant, and potentially transformative, these models are.”
Luis Williams, whose Ph.D. thesis in HSCRB was the first major step in this study, added, “Because we had pluripotent stem cells of human origin, we could make cells in a dish that are relevant to ALS and investigate this very specific problem in the right context: with a human genome and all of the genetic factors that regulate motor neurons.” Williams is now Director of Cell Biology at the biotech startup Q-State Biosciences.
Why it matters
“These experiments point towards a clear path for testing whether repairing Stathmin2 in patients can slow or stop their disease,” explained Eggan. “The discovery we have made suggests a clear approach for developing a potential therapy for ALS – one that would intervene in all but a very small number of individuals, regardless of the genetic cause of their disease.”
The generosity of patients
The mutations in this study are very rare, so the findings were possible thanks to the generosity of patients who donated their own biological samples to Massachusetts General Hospital (MGH), Columbia University, and Project ALS. These samples were used to create the iPS models.
“We are extremely grateful to patients who support science by donating their tissue, because without them we simply cannot make progress,” added Eggan.