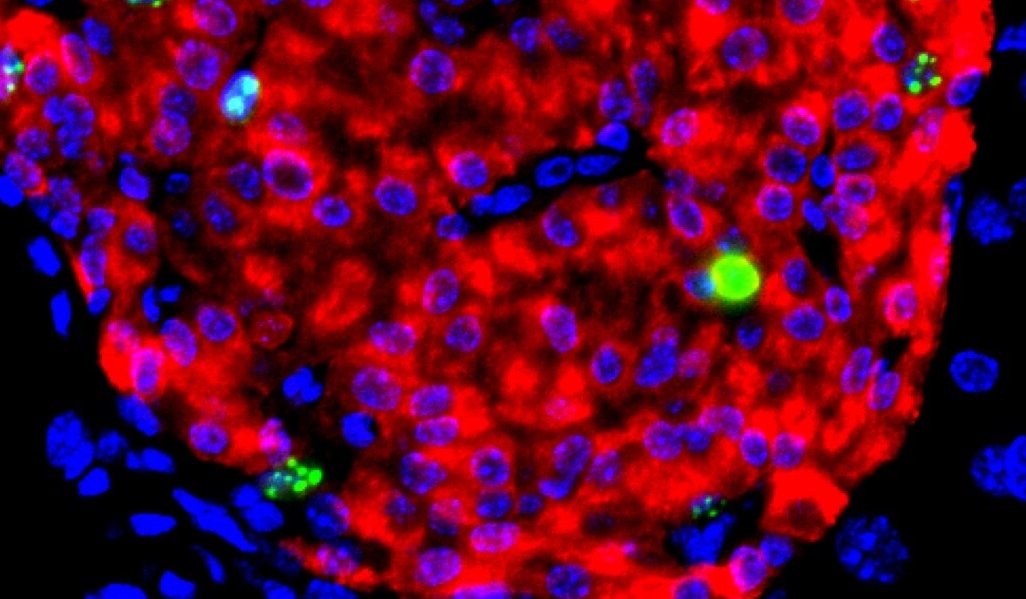
Promising early results show that longstanding research from the lab of Douglas Melton, the Xander University Professor in Harvard’s Department of Stem Cell and Regenerative Biology, may have paved the way for a breakthrough treatment of Type 1 diabetes. Utilizing research from the Melton Lab, Vertex Pharmaceuticals has developed VX-880, an investigational stem cell-derived, fully differentiated pancreatic islet cell replacementtherapy for people with type 1 diabetes (T1D). In conjunction with immunosuppressive therapy, VX-880 produced robust restoration of islet cell function on Day 90 in the first patient in its Phase 1/2 clinical trial.
The patient was treated with a single infusion of VX-880 at half the target dose in conjunction withimmunosuppressive therapy. The patient, who was diagnosed with T1D 40 years ago and has been dependent on injected insulin, achieved successful engraftment and demonstrated rapid and robust improvements inmultiple measures, including increases in fasting and stimulated C-peptide, improvements in glycemic control (HbA1c), and decreases in insulin requirement, which signifies the restoration of insulin-producing islet cells.
This potentially obviates the lifelong need for patients with diabetes to self-inject insulin as the replacement cells “provide the patient with the natural factory to make their own insulin,” said Melton.
VX-880 is not only a potential breakthrough in the treatment of T1D, it is also one of the very first demonstrations of the practical application of embryonic stem cells, using stem cells that have been differentiated into functional islets to treat a patient, said Melton, an Investigator of the Howard Hughes Medical Institute and co-director of the Harvard Stem Cell Institute (HSCI), which partially funded the research. Unlike prior treatments, this innovative therapy gives the patient functional hormone producing cells that control glucose metabolism. “This is an inspiring result, and a wonderful example for how a scientific vision built on basic science developed into a treatment that may profoundly impact the lives of millions of patients,” said Paola Arlotta, Ph.D., the Golub Family Professor and Chair of the Department of Stem Cell and Regenerative Biology.
These results from the first patient treated with VX-880 are unprecedented. “What makes these results truly remarkable is that they were achieved with only half the target dose,” said Bastiano Sanna, Ph.D., ExecutiveVice President and Chief of Cell and Genetic Therapies at Vertex. “While still early, these results support thecontinued progression of our VX-880 clinical studies, as well as future studies using our encapsulated isletcells, which hold the potential to be used without the need for immunosuppression.”
“As a surgeon who has worked in the field of islet cell transplantation for decades, this approach, whichobviates the need for an organ donor, could be a game changer,” said James Markmann, M.D., Ph.D.,Professor of Surgery and Chief of the Division of Transplant Surgery at Massachusetts General Hospital. “We are excited to progress this unique and potentially transformative medicine through clinical trials and to patients.”
“More than a decade ago our lab had a vision for developing an islet cell replacement therapy to provide a functional cure to people suffering from T1D,” said Melton. “These promising results bring great hope that stem cell-derived, fully differentiated islet cells could deliver a life-changing therapy for people who suffer from the relentless life-long burden of T1D.”
Support for this research was provided by the Harvard Stem Cell Institute.